Contraceptives are methods or devices used to prevent pregnancy by interfering with the process of conception or fertilization. They come in various forms and offer different levels of effectiveness. Some common types of contraceptives include:
- Barrier Methods: These include male and female condoms, diaphragms, and cervical caps. Barrier methods physically block sperm from reaching the egg.
- Hormonal Methods: These methods use hormones to prevent ovulation or thicken cervical mucus, making it difficult for sperm to reach the egg. Examples include birth control pills, patches, injections, vaginal rings, and hormonal intrauterine devices (IUDs).
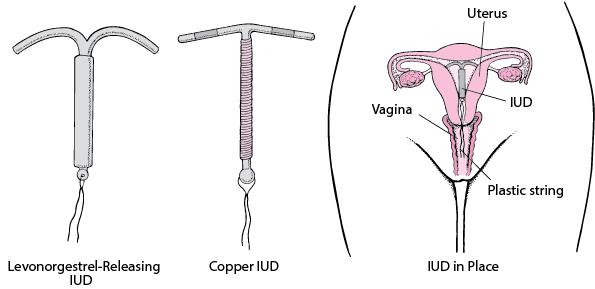
- Intrauterine Devices (IUDs): These are small, T-shaped devices inserted into the uterus to prevent pregnancy. They can be hormonal or non-hormonal and provide long-term contraception.
- Emergency Contraception: Also known as the “morning-after pill,” emergency contraception can be taken within a few days after unprotected intercourse to prevent pregnancy.
- Sterilization: This involves permanent methods such as tubal ligation (for women) or vasectomy (for men) to block or cut the fallopian tubes or vas deferens, respectively.
It’s important to note that contraceptives are intended for pregnancy prevention and do not protect against sexually transmitted infections (STIs). To prevent STIs, it’s advisable to use barrier methods like condoms in addition to other contraceptives.
Remember, if you have specific questions or concerns about contraceptives, it’s always best to consult with a healthcare professional or a qualified provider who can provide personalized advice based on your individual circumstances.
Intrauterine device (IUD).
An intrauterine device (IUD) is a small, T-shaped device that is inserted into the uterus to provide long-term contraception. It is one of the most effective forms of reversible birth control available. Here are some key points to know about IUDs:
Types of IUDs:
There are two main types of IUDs available:
- Hormonal IUDs: These contain progestin, a synthetic form of the hormone progesterone. They release a steady low dose of progestin, which thickens cervical mucus, thins the uterine lining, and in some cases, prevents ovulation. Examples include Mirena, Kyleena, Liletta, and Skyla.
- Copper IUDs: These do not contain hormones. Instead, they are wrapped in a copper wire or have copper sleeves. Copper is toxic to sperm, preventing them from reaching and fertilizing an egg. ParaGard is a commonly used copper IUD.
Effectiveness: Both hormonal and copper IUDs are highly effective at preventing pregnancy. Hormonal IUDs have a failure rate of less than 1%, while copper IUDs have a failure rate of around 0.8%. Once inserted, IUDs can provide contraception for several years, depending on the specific type.
Insertion and Removal: IUD insertion and removal should be performed by a healthcare professional. The process involves placing the IUD into the uterus through the cervix. Some people may experience mild discomfort or cramping during the insertion process. IUDs can be removed at any time if desired, and fertility typically returns quickly after removal.
Benefits: IUDs offer several benefits, including long-term contraception without requiring daily or frequent action. They are highly effective, reversible, and convenient. Hormonal IUDs can also help reduce menstrual bleeding and cramps for some individuals.
Considerations: While IUDs are generally safe, there are a few considerations to keep in mind. Common side effects may include irregular bleeding or spotting, cramping, and in the case of hormonal IUDs, changes in menstrual bleeding patterns. Serious complications are rare but can include perforation of the uterus during insertion or increased risk of pelvic inflammatory disease (PID), especially in the first few weeks after insertion.
It’s important to consult with a healthcare professional to determine if an IUD is the right contraceptive option for you. They can provide personalized advice and address any concerns you may have.
Which one is the safest and most effective.
Both hormonal and copper IUDs are highly effective methods of contraception, but they have different safety profiles. The effectiveness of both types of IUDs is comparable, with failure rates of less than 1%. However, the safety considerations and side effects differ between them.
Hormonal IUDs (e.g., Mirena, Kyleena, Liletta, Skyla) have the following characteristics:
- Safety: Hormonal IUDs are generally safe and well-tolerated. However, they may not be suitable for individuals with certain medical conditions, such as liver disease or certain types of cancer.
- Side Effects: Hormonal IUDs can cause changes in menstrual bleeding patterns. Some people experience lighter periods or even stop having period’s altogether, while others may experience irregular bleeding or spotting, especially during the first few months of use. Hormonal IUDs may also cause hormonal side effects such as breast tenderness, mood changes, or acne, although these effects are usually minimal due to the low hormone dose.
- Additional Benefits: Hormonal IUDs can offer additional benefits beyond contraception. They are often prescribed to individuals with heavy or painful periods because they can help reduce menstrual bleeding and cramps.
Copper IUDs (e.g., ParaGard) have the following characteristics:
- Safety: Copper IUDs do not contain hormones and are considered safe for most individuals, including those who cannot use hormonal contraceptives.
- Side Effects: Copper IUDs may lead to heavier and more prolonged menstrual bleeding and may cause increased cramping during periods. However, these side effects tend to diminish over time for many individuals.
- Non-Hormonal: The copper IUD is a non-hormonal option, which means it does not have the potential hormonal side effects associated with hormonal contraceptives.
Ultimately, the choice between a hormonal or copper IUD depends on factors such as personal preference, medical history, and individual needs. It’s important to discuss your options with a healthcare professional who can provide personalized advice based on your specific circumstances and help you determine which IUD may be the safest and most suitable for you.
Can You Take Contraceptives after Birth?
Yes, contraceptives can be used after giving birth to prevent subsequent pregnancies. The timing of when you can start using contraceptives after birth depends on various factors, including whether you are breastfeeding and the type of contraceptive method you plan to use. Here are some options:

- Barrier Methods: Barrier methods, such as condoms or diaphragms, can be used immediately after giving birth. They do not have any hormonal effects and can be used regardless of breastfeeding status.
- Progestin-Only Contraceptives: Progestin-only contraceptives, including the mini-pill (progestin-only birth control pill), progestin-only implants (such as Nexplanon), or progestin-only injections (such as Depo-Provera), can usually be initiated shortly after birth, even while breastfeeding. It’s important to consult with a healthcare professional to determine the appropriate timing based on individual circumstances.
- Combined Hormonal Contraceptives: Combined hormonal contraceptives, such as birth control pills that contain both estrogen and progestin, or the contraceptive patch or vaginal ring, are generally not recommended immediately after giving birth, especially if you are breastfeeding. Estrogen in these methods may interfere with milk supply. However, they can typically be started after around 4-6 weeks postpartum, once breastfeeding is well-established and your body has had time to recover.
- Intrauterine Devices (IUDs): Both hormonal and copper IUDs can be inserted immediately after childbirth, including right after delivery or during a cesarean section. This is known as immediate postpartum insertion. Copper IUDs can be used regardless of breastfeeding status. Hormonal IUDs are also safe to use while breastfeeding.
It’s important to discuss your contraceptive options with your healthcare provider to determine the most appropriate method for you after giving birth.
They can provide guidance based on your specific circumstances, preferences, and individual health factors.
Contraceptives after an Abortion,
After an abortion, it’s important to consider contraception to prevent future pregnancies if that is your intention. The timing of when you can start using contraceptives after an abortion depends on the type of abortion procedure and individual circumstances. Here are some general guidelines:

- Surgical Abortion: If you underwent a surgical abortion, your healthcare provider will provide guidance on when it is safe to start using contraception. In many cases, contraception can be initiated immediately after the procedure.
- Medication Abortion: If you had a medication abortion (using medication to induce abortion), the timing may vary. It’s essential to follow the instructions provided by your healthcare provider regarding when you can start using contraception after the medication abortion.
The contraceptive options available after an abortion are generally similar to those available in other situations. These options include barrier methods (condoms, diaphragms), hormonal methods (birth control pills, patches, injections, hormonal IUDs), and copper IUDs. The choice of method depends on your individual needs, preferences, and medical history.
It’s advisable to discuss your contraceptive options with your healthcare provider after an abortion. They can provide personalized advice and help you choose the most suitable contraceptive method based on your specific circumstances and future pregnancy plans.
IUD Failure.
While IUDs are highly effective at preventing pregnancy, like any contraceptive method, they are not 100% foolproof and can occasionally fail. However, the failure rate of IUDs is very low. Here are some reasons why an IUD may fail:
- Incorrect Insertion: If the IUD is not properly inserted by a healthcare professional, it may not be positioned correctly in the uterus, reducing its effectiveness. It’s important to have an experienced healthcare provider perform the insertion to minimize this risk.
- Expulsion: In rare cases, the IUD may become partially or fully expelled from the uterus without the person noticing. This can happen due to uterine contractions, especially in the first few months after insertion. Checking for the presence of the IUD’s strings regularly and seeking medical attention if any signs of expulsion occur can help prevent this.
- Displacement: Sometimes, the IUD can shift or move from its ideal position within the uterus. This can potentially reduce its effectiveness. Regular check-ups with a healthcare provider can help detect any displacement and ensure the IUD remains in the correct position.
- Pregnancy prior to IUD insertion: If a person is already pregnant at the time of IUD insertion, the IUD will not prevent that pregnancy. It’s crucial to ensure that you are not pregnant before getting an IUD inserted.
It’s important to note that the failure rate of IUDs is very low, generally less than 1%. They are one of the most effective forms of contraception available. If you have concerns about the effectiveness of your IUD or suspect a failure, it’s best to consult with a healthcare professional who can evaluate the situation and provide appropriate guidance.
You can visit our facility or contact us for guidance.