Emergency contraception (P2).
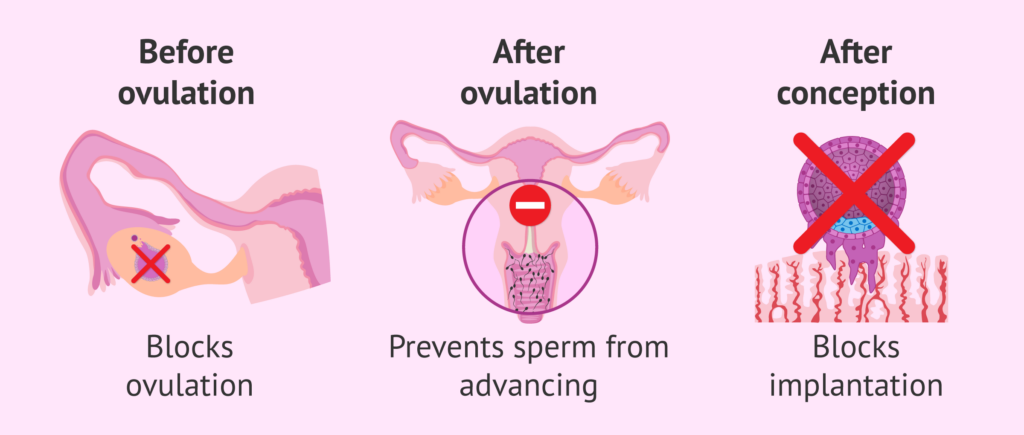
Emergency contraception, commonly known as the “morning-after pill,” is a form of contraception that can be used after unprotected sexual intercourse or contraceptive failure to help prevent pregnancy. It is intended to be used as a backup method and should not replace regular, ongoing contraception.
There are a few different types of emergency contraceptive pills available, but the most common ones contain levonorgestrel or ulipristal acetate as the active ingredients. Here’s some information about each:
- Levonorgestrel pills: These are available over-the-counter without a prescription and are most effective when taken as soon as possible after unprotected sex, ideally within 72 hours (3 days). Some brands require taking two pills, while others require just one. Levonorgestrel works by preventing or delaying ovulation.
- Ulipristal acetate pills: This type of emergency contraception requires a prescription. It is effective up to 120 hours (5 days) after unprotected sex. Ulipristal acetate works by inhibiting or delaying ovulation.
It’s important to note that emergency contraception is not as effective as regular forms of contraception, such as birth control pills or condoms. It should be used only in emergency situations and not as a primary method of contraception.
Effectiveness of emergency contraception
The effectiveness of emergency contraception can vary depending on several factors, including the type of emergency contraceptive used and the timing of its administration. Here’s a general overview of the effectiveness rates:
- Levonorgestrel pills: When taken within 72 hours (3 days) after unprotected sex, levonorgestrel emergency contraceptive pills are estimated to prevent approximately 85% of pregnancies that would have otherwise occurred. However, their effectiveness decreases over time, so taking them as soon as possible after unprotected sex is crucial.
- Ulipristal acetate pills: When taken within 120 hours (5 days) after unprotected sex, ulipristal acetate emergency contraceptive pills are estimated to be more effective than levonorgestrel, preventing approximately 98% of pregnancies that would have otherwise occurred.
It’s important to understand that emergency contraception is not 100% effective and should not be relied upon as a primary method of contraception. Regular, ongoing contraception methods, such as birth control pills, patches, implants, or condoms, are more effective for preventing pregnancy when used consistently and correctly.
Additionally, emergency contraception does not protect against sexually transmitted infections (STIs). If there is a risk of STIs, it’s essential to use barrier methods, such as condoms, in addition to emergency contraception.
If you have concerns about the effectiveness of emergency contraception or need further information, it’s recommended to consult a healthcare professional who can provide personalized advice and guidance based on your individual circumstances.
What is the next step after their failure?
If you have taken emergency contraception and suspect that it may have failed, or if you experience symptoms of pregnancy after taking it, it is important to take the following steps:
- Take a pregnancy test: If you have missed your period or are experiencing symptoms of pregnancy, such as breast tenderness, nausea, or fatigue, take a pregnancy test to confirm whether you are pregnant or not. Home pregnancy tests are readily available at pharmacies and are typically reliable when used correctly.
- Consult a healthcare professional: If the pregnancy test confirms that you are pregnant or if you have concerns about the effectiveness of emergency contraception, it is recommended to consult a healthcare professional, such as a doctor or a gynecologist. They can provide guidance, conduct further tests if necessary, and discuss your options moving forward.
- Discuss contraception options: If you are not ready for a pregnancy, your healthcare provider can discuss various contraceptive methods with you. They will consider factors such as your overall health, reproductive goals, and personal preferences to help you choose a reliable and suitable contraceptive method.
- Consider additional emergency contraception: Depending on the situation, your healthcare provider may discuss alternative emergency contraception options, such as the copper IUD. The copper IUD can be inserted by a healthcare professional up to five days after unprotected sex and is highly effective at preventing pregnancy.
Remember, the effectiveness of emergency contraception can vary, and it is not a guarantee against pregnancy. It is always advisable to use regular and consistent contraception methods to minimize the risk of unintended pregnancies.
What happens after failed contraception does it affect the pregnancy.

If a contraceptive method fails and pregnancy occurs, it’s important to note that the failed contraception itself does not typically have any direct impact on the pregnancy. Once fertilization has occurred, the pregnancy progresses independently of the contraceptive method.
The potential risks or effects on the pregnancy would depend on various factors, such as the type of contraceptive method used, the timing of its failure, and any potential underlying health conditions. For example:
- Hormonal contraceptives (such as birth control pills, patches, or injections): If pregnancy occurs despite the use of hormonal contraceptives, discontinuing the contraceptive method is generally advised. However, hormonal contraceptive use early in pregnancy (before a woman realizes she is pregnant) is not known to increase the risk of adverse effects on the pregnancy or the fetus.
- Intrauterine devices (IUDs): In most cases, if a pregnancy occurs with an IUD in place, the IUD should be removed. The timing and method of removal would depend on the specific circumstances, and it is typically recommended to consult with a healthcare professional promptly.
- Barrier methods (such as condoms or diaphragms): If a barrier method fails, there are generally no direct effects on the pregnancy. However, it is important to evaluate the potential risk of sexually transmitted infections (STIs) if the barrier method failed.
In any case, if you suspect that a contraceptive method has failed and you are pregnant or have concerns about the pregnancy, it is crucial to consult with a healthcare professional. They can provide proper evaluation, guidance, and necessary care throughout the course of the pregnancy to ensure the best possible outcome for both the mother and the baby.
Common pregnancy symptoms.
Common pregnancy symptoms can vary from person to person, and not all individuals experience the same symptoms or severity. However, here are some common early pregnancy symptoms:
- Missed period: One of the most common signs of pregnancy is a missed menstrual period. However, it’s important to note that missed periods can also occur due to other factors, such as stress, hormonal imbalances, or certain medical conditions.
- Breast changes: Many women experience breast changes early in pregnancy. This can include increased sensitivity, tenderness, swelling, or changes in the nipples.
- Fatigue: Feeling more tired or fatigued than usual is a common early pregnancy symptom. This can be attributed to hormonal changes in the body.
- Nausea and vomiting (morning sickness): Nausea, sometimes accompanied by vomiting, is commonly referred to as morning sickness. However, it can occur at any time of the day. Not all pregnant individuals experience morning sickness, and the severity can vary.
- Frequent urination: Increased frequency of urination is a common symptom due to hormonal changes and increased blood flow to the kidneys during pregnancy.
- Food cravings or aversions: Some pregnant individuals may experience cravings for certain foods or develop aversions to foods they previously enjoyed.
- Mood swings: Hormonal fluctuations during pregnancy can lead to mood swings, irritability, or emotional changes.
- Changes in the sense of smell: Heightened sensitivity to certain smells or aversion to strong odors is another common symptom.
It’s important to note that these symptoms can also be caused by factors other than pregnancy. If you suspect you may be pregnant or are experiencing these symptoms, it is recommended to take a pregnancy test or consult with a healthcare professional for an accurate diagnosis and appropriate guidance.
Pregnancy complication.
Pregnancy can be a joyful and exciting time, but it can also come with potential complications. Some common pregnancy complications include:
- Gestational diabetes: This is a type of diabetes that develops during pregnancy. It is characterized by high blood sugar levels and usually resolves after delivery. Proper management is important to prevent complications for both the mother and the baby.
- Pre-eclampsia: Pre-eclampsia is a condition characterized by high blood pressure and damage to organs, typically the liver and kidneys. It usually occurs after the 20th week of pregnancy and can affect both the mother and the baby. Regular prenatal care is crucial for early detection and management.
- Miscarriage: Miscarriage refers to the loss of a pregnancy before the 20th week. It can occur due to various factors, including genetic abnormalities, hormonal imbalances, or maternal health conditions. If you experience vaginal bleeding, abdominal pain, or cramping during pregnancy, it’s important to seek medical attention.
- Ectopic pregnancy: An ectopic pregnancy occurs when the fertilized egg implants outside the uterus, most commonly in the fallopian tubes. It is a potentially life-threatening condition that requires immediate medical intervention.
- Placenta previa: Placenta previa is a condition in which the placenta partially or completely covers the cervix, leading to bleeding during pregnancy. It may require monitoring or intervention to ensure the safety of both the mother and the baby.
- Preterm labor: Preterm labor refers to the onset of labor before 37 weeks of gestation. Premature babies may have health complications due to their underdeveloped organs and require specialized care.
- Fetal growth restriction: Fetal growth restriction occurs when the baby does not grow at the expected rate during pregnancy. It can be caused by various factors, including placental problems, maternal health conditions, or genetic factors. Regular prenatal check-ups can help monitor the baby’s growth and well-being.
It’s important to remember that not all pregnancies will experience complications, and many pregnancies progress without major issues